Certain socioeconomic and sociodemographic factors make individuals more likely to suffer from long COVID, according to a preprint study (PDF) by Daniel Kim, M.D., of the School of Public Policy and Urban Affairs at Northeastern University.
Predictors of long COVID risk include lower household income, being divorced or separated, being Hispanic, being female and being gay or bisexual, according to the study, which was posted on medRxiv, a clearinghouse for studies that have not yet been peer reviewed.
Kim found that having long COVID was linked to higher risks of recent unemployment, financial hardship, and anxiety and depression.

Long COVID presents something of a conundrum for payers and the beneficiaries they cover because, at present, there exist no generally agreed upon diagnostic and/or treatment best practice guidelines.
Richard Stefanacci, chief medical officer at the Jefferson College of Population Health at Thomas Jefferson University, told Fierce Healthcare in November that he thinks payers should “keep up to date regarding findings on diagnosis and treatment.”
Public health officials have been criticized for being slow to recognize the dangers posed by long COVID. It wasn’t until June that a national tally started being kept on how many individuals have long COVID, and it wasn’t until August that the U.S. government formalized an action plan to study it.
The Centers for Disease Control and Prevention (CDC) last month said that 3,544 individuals in the U.S. have died from long COVID, but the number is probably much higher.
The CDC’s tally comes from death certificates, and there was no code for death by long COVID until last month. Rather than checking a box, long COVID had to be written in as a cause of death.
Kim’s study represents the largest multivariable analysis to date using a population that mirrors the socioeconomic strata of the U.S. It extracts data from 152,812 adults aged 18 and older of whom 19,871 had long COVID. The data were culled from the U.S. Census Bureau’s Household Pulse Survey (HPS). The national HPS surveys were sent out three times from Sept. 14, 2022, through Nov. 14, 2022.
According to Kim’s findings, about 14% of U.S. adults aged 18-84—anywhere from 33.63 million to 35.47 million individuals—suffer from long COVID. Those saying that they experienced a modest impact or considerable impact on daily functioning because of long COVID accounted for 57.2% and 21.8%, respectively. As many as 28.02 million adults in the U.S. could currently have long COVID, of whom as many as 25.3 million would be working-aged, according to the study.
“Given that cases of COVID will continue to accrue from new infections and re-infections in the ongoing pandemic, these numbers of susceptible individuals will only escalate over time,” the study said. “The preliminary findings from this study highlight the anticipated substantial health and economic burden of long COVID among American adults. Should these estimates be confirmed in longitudinal studies, future efforts should focus on identifying biological and social explanations and mediating pathways for associations, and on targeting risk reduction in those at higher risk of long COVID."
COVID-19’s ability to mutate continues to present challenges to the healthcare system, which is facing the rise of XBB.1.5, a subvariant of omicron.
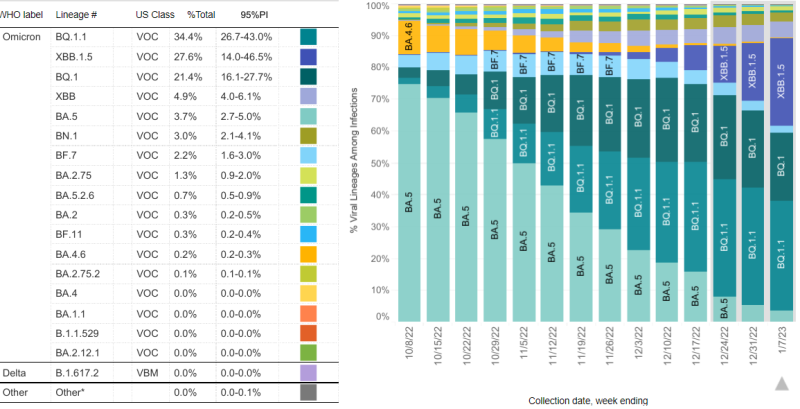
XBB 1.5 accounted for 27.6% of new cases of COVID-19 as of the week ending Jan. 7, 2023; that’s up from 18.3% from the prior week, according to the CDC.
Kim’s study said that “receipt of a COVID-19 vaccine (with or without a booster) was linked to lower risks of COVID-19 infection.” On the other hand, “those who completed their primary vaccination series but did not receive the vaccine booster had a higher risk of long COVID than the unvaccinated. … While adjustment was made for receipt of a COVID-19 vaccine booster due to a COVID-19 infection, residual confounding due to indication could explain the null and positive associations between vaccination against COVID-19 and long COVID.”
Kim said his findings indicate the potential for substantial health and economic burden because of long COVID.
“Should these estimates be confirmed in longitudinal studies, future efforts should focus on identifying biological and social explanations and mediating pathways for associations, and on targeting risk reduction in those at higher risk of long COVID,” the study said. “Candidate interventions to mitigate adverse health and economic sequelae of long COVID could include enhanced uptake of COVID-19 vaccines by higher-risk groups to reduce the risk of acute COVID-19 infection and expanded access to paid sick leave and disability insurance.”