Experts believe recent price transparency initiatives from the Centers for Medicare & Medicaid Services (CMS) are a step in the right direction but ultimately fall short of making the impact all parties desire.
In July, CMS proposed that all hospitals must use a standard template in a machine-readable file format. Health payers already follow this requirement. The rule, which would go into effect March 1 if approved, would also look to align and combine other price transparency efforts strewn across the No Surprises Act and the Transparency in Coverage regulation.
The proposal offers data on cost and value differences between health plans and hospitals. In a perfect world, price transparency allows consumers to look up and compare the cost of medical services before being taken off guard.
“We view this as a big win to continue on the path of price transparency,” said Carol Skenes, a provider and payer specialist for Turquoise Health, a software solutions healthcare company based in San Diego.
Turquoise Health CEO Chris Severn testified before Congress this year, arguing for the importance of standardized schema in medical forms, machine-readable files and consolidated hospital information.
For hospitals, there is no standardized schema, explained Skenes, so about 6,000 hospitals have their own variations of forms. Under the new proposal, thousands of files can be modified to fit one format and should be easily replicated in the future.
CMS guidelines would require hospitals to post additional verbiage so consumers can know when a file was last updated and where to find a file on the hospital’s website and requires them to add additional columns to make reporting simpler by defining rate types.
“So, if you’re comparing $5,000 to $20,000, but you have no context of whether one is paid once per day or if one is paying for a week’s worth stay, it’s not really an apples-to-apples comparison,” Skenes told Fierce Healthcare. She said that since some contract structures are based on algorithms, this price transparency proposal would give more clarification on how percentages of charges will impact a patient’s bill because hospitals will come up with an average expected price.
The proposal's impact could be limited
While the CMS proposal should become more transparent for the average consumer, it’s likely that it won’t benefit as many consumers as needed to be a transformative shift for the industry, experts say.
According to Trilliant Health CEO Hal Andrews, only 12% of all healthcare encounters happen at hospitals and half of those admissions originate in an emergency department, leaving only planned visits as a chance to take advantage of hospital price transparency. As a result, he believes the hospital price transparency data have less utility than the health plan price transparency, and the proposed rule only offers value if you have a planned upcoming hospital admission, easily identifiable shopping objectives and nothing unplanned pops up once there. Hospital price transparency also does not include the cost of services in ambulatory care settings.
“Even if hospitals comply perfectly with what is included in the [Outpatient Prospective Payment System (OPPS)] proposed rule, hospital price transparency will not cover almost 90% of healthcare encounters, many of which are more likely to be 'shopped' by consumers,” he said. “On the other hand, health plan price transparency data includes a 100% sample, allowing consumers to search for any and every service covered by their insurance.”
A normal hospital chargemaster has about 40,000 to 50,000 items, he added, but hospitals are only required to post consumer-friendly descriptions for around 300 items. That number would rise to about 500 if the proposed rule goes through, a small percentage of total chargemaster items. Even if all chargemaster items were given a description outside of medical nomenclature, the average consumer would still struggle to make sense of everything, although generative artificial intelligence could start to help translate medical definitions.
“For surgical patients, it would be impossible to know in advance how much anesthesia or blood would be required intra-operatively, nor would a patient know how much pain medicine they would receive,” Andrews said. “I think the notion that consumers should understand what they’re paying for is the right notion. I think that it’s easy to publish a rule and say, 'Everybody post this stuff.’ I’m stunned that nobody’s figured out that the average American wouldn't have any way to consume this data. It’s like a foreign language. Even if you brought in a physician, the physician may only know a handful of codes relevant to them, but there are thousands and thousands of codes.”
“I think my issues are more that this is typical of people in the beltway doing stuff and not really understanding how the world works,” he added.
Emergency department visits only occur when there is an urgent medical need. Both Andrews and Skenes agreed that price transparency data won’t be useful in those situations either, because patients won’t be comparing rates when medical care is the most time-sensitive.
“You couldn’t proactively research emergency situations,” said Skenes, noting that she also thought it’s an “unreasonable expectation” to assume the average consumer will be able to navigate machine-readable files and predict upcoming services.
Health plan price transparency data show value
Analysis from Trilliant that combines Hospital Readmissions Reduction Program data with additional data from its provider directory and health plan price transparency dataset shows that within a single healthcare plan for each hospital, rate variance can be up to eight times different, or more costly, despite tightly correlated quality of care, depending upon the operation.
Patients looking for a hip and knee replacement in the surrounding Chicago area could expect to pay around $20,000 to $80,000, but there is a slightly negative correlation between price and quality for this operation, meaning care slightly decreases per dollar spent on average, according to the data. Quality of care is consistent for other procedures, including acute myocardial infarctions, COPD, heart failure or pneumonia, even though the cost can vary drastically.
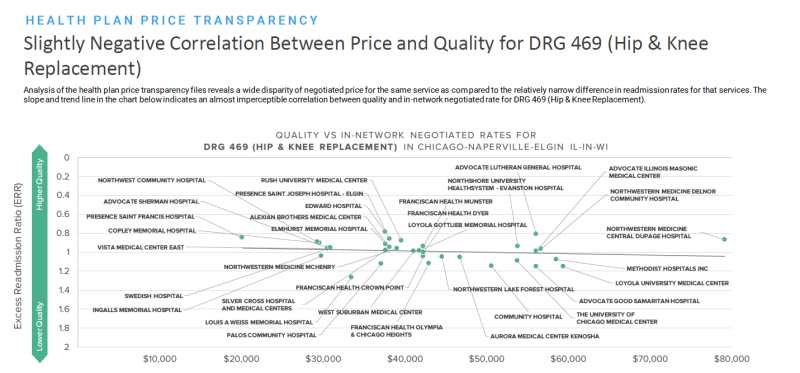
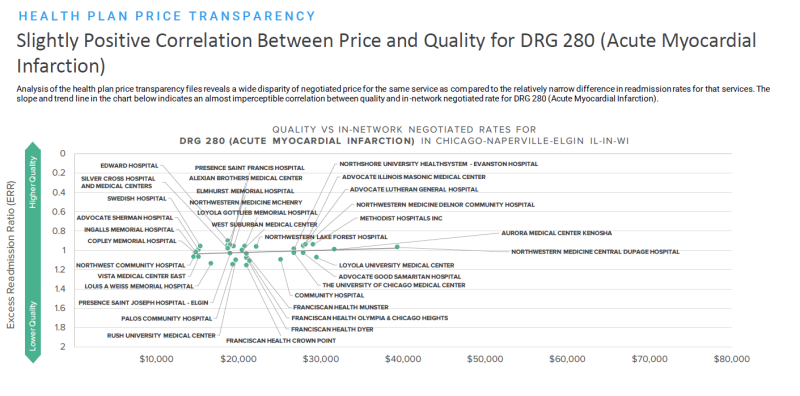
“In terms of value, or where can I get the best price for equivalent quality, it’s stunning how these things jump off the page,” said Andrews. “What you see in the data is that nobody is good at everything, and you don’t have to steer away from a single provider, you just have to steer away from one or two.”
“We’re seeing a lot of data validation occur of comparing rates between the hospital data and the payer data,” said Skenes. “Ideally, those rates match, which gives the users in the industry a lot more confidence that the rates that are getting posted are accurate.”
Whether the OPPS proposal goes far enough in showing the average consumer the power of price transparency tools, there’s clear potential for more transparency in the future, she said.
“If you know if every single hospital machine-readable file came in the standard schema tomorrow, that still wouldn’t be the end of the line for price transparency,” Skenes explained. “There’s a lot more work to be done to make sure patients understand bundles and how to look at all these different items and services.”
Skenes expects upcoming efforts will evolve around consolidating requirements at the federal level, as well as simplifying estimates for patients, hospitals and insurers.