Treating substance use disorders costs employer-sponsored insurance $35.3 billion a year, with alcohol and opioid misuse topping the list of what many working-age people struggle with, according to a study by researchers with the Centers for Disease Control and Prevention (CDC).
Employers should install programs to help employees address these problems, because the costs most likely balloon when factoring in residual effects such as presenteeism, absenteeism and job retention, according to the study, published today in JAMA Network Open.

The study’s corresponding author, Cora Peterson, Ph.D., a senior health economist at the CDC’s Division of Injury Prevention at the Injury Center, told Fierce Healthcare that employers can find different approaches to battling substance use disorders on the Workplace Supported Recovery Program (WSRP) webpage. The cite is run by the National Institute for Occupational Safety and Health, which is a division of the CDC.
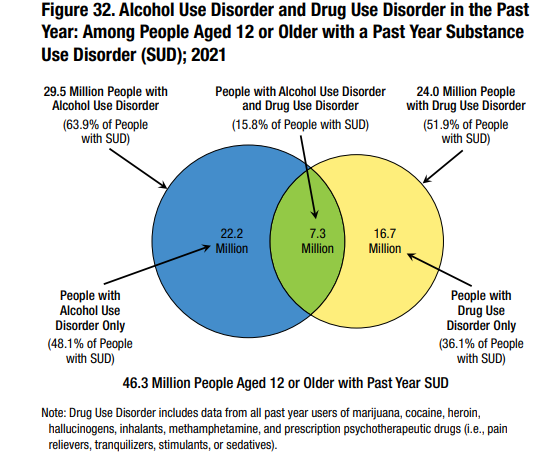
The site notes that about 70% of adults with alcohol or drug problems work. “Nearly 9% of all employed adults (approximately 13.6 million workers) have current alcohol or illicit drug use disorders, while a relatively equal number (approximately 13.4 million workers) report that they are in recovery or have recovered from a substance use problem,” the WSRP webpage said.
Peterson added that “given the substantial annual direct medical cost that SUD incurs in the U.S. population with employer-sponsored health insurance, all employers and health insurance payers can consider the potential cost-effectiveness of prevention and treatment strategies.”
Ellen Kelsay, president and CEO of the Business Group on Health, said she couldn’t agree more and states that SUD represents a significant concern for employers.
“There are several considerable challenges to supporting people with SUD that include a dearth of expert providers in many communities and an ongoing stigma against those with SUD,” Kelsay told Fierce Healthcare. “Many fear losing their job if they self-report SUD, so people may be less likely to seek treatment of support from their workplace. Treatment can be costly, especially for inpatient care.”
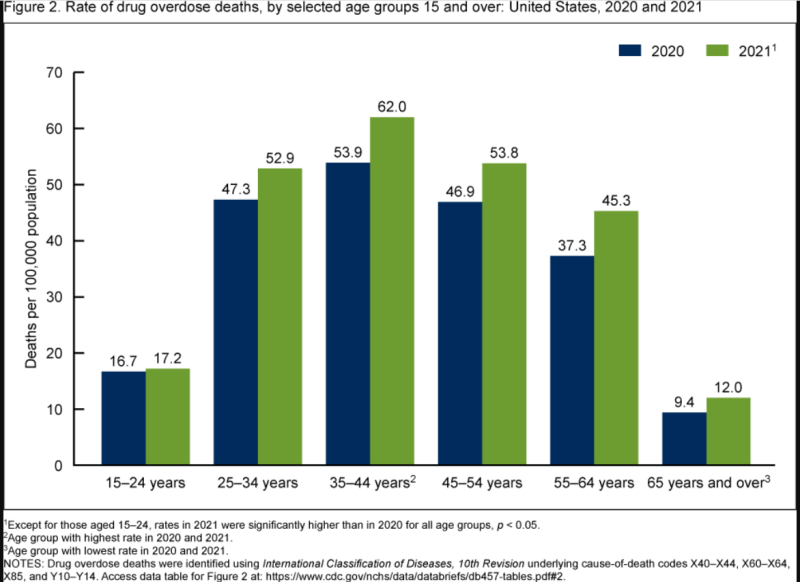
Most overdose deaths occur among working-age individuals; over 70% were 25 to 34 years old in 2020, said Kelsay, adding that “employers are implementing anti-stigma campaigns; manager- and peer-support trainings, and first-incident ‘forgiveness’ policies to increase the likelihood that people access medical treatment for their SUD.”
Kelsay adds that:
- The number of employers offering Centers of Excellence for SUD jumped from 20% in 2022 to 34% in 2023, and another 19% might implement it in 2024, according to the Business Group's annual employer survey.
- Virtual care programs that bring treatment into the home have shown good initial results.
- Some companies have reduced or eliminated cost sharing for mental health services.
- Employers are stocking up on Narcan and training employees how to use it to stop an overdose in the workplace.
Randa Deaton, the vice president of purchaser engagement at the Purchaser Business Group (PBHG) on Health, tells Fierce Healthcare that, employers’ concern about mental health treatment for employees focus mainly on access to care.
“One of the biggest challenges employers face with regard to substance use disorder is that primary care doesn’t routinely screen for these disorders or make referrals to appropriate care,” says Deaton. “The second big challenge is that there are a lot of substance use disorder programs that are not grounded in evidence-based approaches but rather abstinence-based programs that don’t include medical assisted treatment.”
PBGH comprises about 40 large private and public employers who spend about $350 billion a year to cover 21 million Americans. Deaton says some member companies have started using onsite employee assistance program counselors “that help make referrals for workers and are increasingly using new virtual models of MH/SUD to increase access to care.”
The JAMA Network Open study found that “the $35.3 billion SUD medical cost represents a small fraction of total U.S. personal health care expenditures paid by private insurance ($1.1 trillion in 2018)."
However, while the estimated annual cost of treating SUDs comes to $15,640 per affected enrollee, only 1% of employer plan members are diagnosed with SUD, while 11% of workers self-report that they battle SUD, suggesting much higher costs for employers and the health insurance plans that they contract with than this study reflects.
“The cost of strategies to support employees and their health insurance dependents to prevent and treat SUDs can be considered in terms of potentially offsetting the existing high medical cost of SUDs,” the study concluded. “Medical expenditures for SUDS represent the minimum direct cost that employers and health insurers face because not all people with SUDs have a diagnosis, and costs related to absenteeism, presenteeism, job retention and mortality are not addressed.”

Kelsay says that “when someone has a child or family member suffering from SUD, it can have a significant impact on their ability to focus at work; cause additional financial hardship; reduce their own job retention; and increase the likelihood of anxiety, depression and related health issues.”
Among employer plan members with a SUD diagnosis, alcohol-related disorders ($10.2 billion—or about 50% of total cost) and opioid-related disorders ($7.3 billion—or about 30% of total cost) were the most expensive.
The average annual cost per enrollee for inpatient treatment of alcohol use disorder was from $3,837 to $4,140; and for opioids from $3,336 to $3,804. The average annual cost for outpatient treatment for the two was from $4,716 to $5,033 for alcohol, and $5,976 to $6,585 for opioids. Overall, for alcohol from $8,680 to $9,197, and for opioids from $11,317 to $12,424.
Among enrollees with a SUD diagnosis, the most common comorbidities were depression (30%), hypertension (29.8%) and obesity (17%).
CDC researchers examined employer plan data from Jan. 1 to Dec. 31, 2018, analyzing the information from January to March 2022. Of the 162 million enrollees, 2.3 million (1.4%) had been diagnosed with an SUD in 2018. The data were mined from about 350 payers, including large employers, health insurers and the government.
Substance use disorder can involve alcohol, cannabis, hallucinogens, inhalants, opioids, sedatives and stimulants.
By comparing total annual medical expenditures among similar enrollees with and without an SUD diagnoses, “this analysis aimed to estimate the cost that could be eliminated through prevention or successful treatment of SUD,” the study said.
“Successful treatment” presents a challenge.
About 90% of alcoholics will relapse within four years, according to the National Institute on Alcohol Abuse and Alcoholism. One study found that 91% of people with opioid addictions relapsed after getting sober, and 54% of those relapsed within one week.
In response, Kelsay said, many employers:
- Provide a SUD benefit that steers individuals and their families to high quality care.
- Create a workplace culture that eliminates stigma and encourages individuals to seek care.
- Empower telehealth treatment for workers who don’t go to the office.
- Allow flexibility that lets workers get the treatment and support that they need during the workweek.
The CDC researchers in the JAMA Open Network study addressed not just the cost difference between patients in hospitals who may or may not have had a SUD diagnosis as a primary reason for seeking care but also among patients who went to the hospitals for other reasons, such as heart problems.
The comparisons considered patients with the same demographic characteristics, health plan type and comorbidities, but who did not necessarily have SUD.
“By comparing total annual medical expenditures among similar enrollees with and without SUD diagnoses (referred to as control participants), this analysis aimed to estimate the cost that could be eliminated through prevention or successful treatment of SUD (referred to as the attributable cost),” the study said.