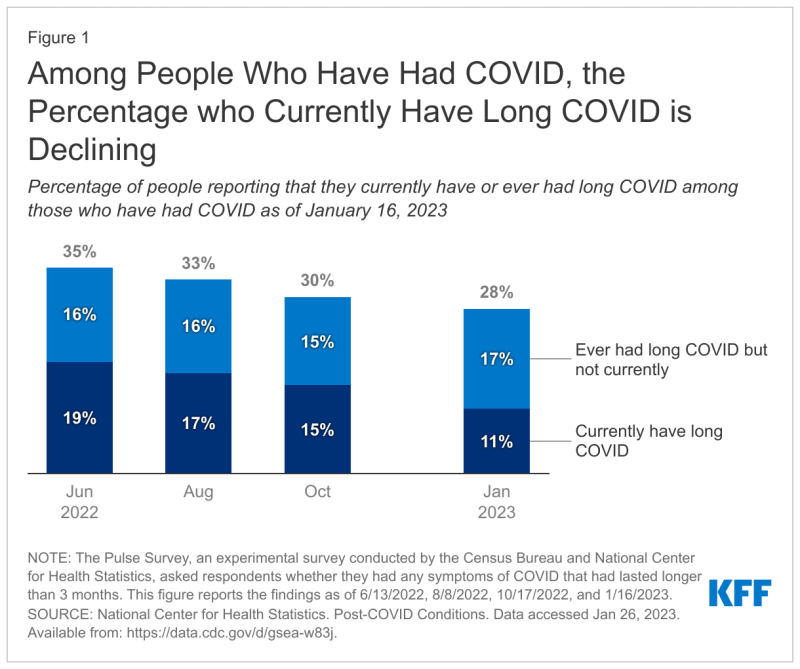
The percentage of individuals who’ve had COVID-19 and then wind up with long COVID shrank from 19% in June 2022 to 11% this month, according to a report by the Kaiser Family Foundation, which analyzed data from the Centers for Disease Control and Prevention (CDC).
“That decrease reflects a reduction in the share of people who have COVID and later report long COVID, which declined from 35% to 28% during the same period," researchers at KFF wrote.
Some health insurance plans and employers who self-insure might breathe a sigh of relief about this development. Even though generally agreed-upon best practices for diagnosing and treating long COVID have yet to be adopted, the condition looms large for payers as a possible future cost burden.
Elizabeth Mitchell, the president and CEO of the Purchaser Business Group on Health, told Fierce Healthcare last November that group members recognize long COVID will not only impact cost, but “employee health and wellbeing. I think there’s a big unknown about what the impact is going to be, but there is at least acknowledgment that there will be an impact and that employers are going to have to adjust.”
The KFF study analysis also alludes to the “big unknown,” stating that “there is still a great deal of uncertainty about long COVID and whether there will be increased long COVID cases following the holiday bump.”
Many people with long COVID have difficulty finding the care that they need, often having to visit a multitude of specialists, according to the KFF analysis.
The CDC said, “there is no test that determines if your symptoms or condition is due to COVID-19. Post-COVID conditions are not one illness. Your healthcare provider considers a diagnosis of post-COVID conditions based on your health history, including if you had a diagnosis of COVID-19 either by a positive test or by symptoms or exposure, as well as doing a health examination.”
Meanwhile, providers might have difficulty recommending a course of treatment.
“Among people with activity limitations who are unable to work, many have trouble accessing disability benefits through their workplaces or through federal disability insurance programs,” the KFF analysis said. “Because long COVID is more common among people with lower levels of education, it is likely that people in low-wage jobs without benefits are overrepresented among those unable to work on account of long COVID.”
The tally of individuals in the workforce with long COVID ranges from 500,000 to 4 million, depending on the study.
Still, the KFF study gives reason for hope, noting that while 11% of people who’ve had COVID-19 experience long COVID, 17% of individuals who had long COVID no longer experience any symptoms. “Those numbers suggest that more people have recovered from long COVID than currently report symptoms,” the KFF study said.
Seventy-nine percent of individuals with long COVID say that the condition limits their daily activities, and 27% say it significantly limits their activities.
However, the CDC data KFF analyzed come from the agency’s Household Pulse Survey, which may be an inaccurate reflection of long COVID’s effects.
“On the one hand, it may be difficult for people with severe limitations to respond to the survey, so the survey may undercount people with severe limitations from long COVID,” the KFF analysis said. “On the other hand, people who experience long COVID and especially, limitations from long COVID, may be more likely to respond to the survey, so the survey may overcount people with activity limitations from long COVID.”