The country's largest pharmacy benefit manager is taking a page out of Mark Cuban's book.
Express Scripts on Tuesday announced the launch of its new pharmacy network option, ClearNetwork, which operates under a cost-plus model. In this approach, clients pay a "straightforward" acquisition cost for individual drugs as well as a small markup that covers dispensing and service costs.
ClearNetwork will be available to a range of clients including employers, government organizations and private payers.
"We are constantly innovating to provide our clients with new options that meet their needs and enable them to build custom pharmacy benefits that best support their plans and members," said Adam Kautzner, president of Express Scripts, in the release. "The Express Scripts ClearNetwork leverages our scale, relationships, and deep understanding of the pharmaceutical supply chain to create an easy-to-follow option for clients looking to simplify what they pay for prescription drugs, while supporting a seamless, convenient member experience."
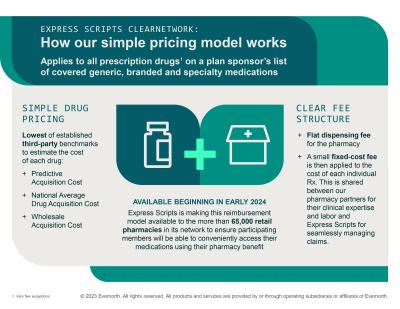
The ClearNetwork model estimates the acquisition cost for individual medications using multiple established third-party benchmarks including predictive acquisition cost, national average drug acquisition cost and wholesale acquisition cost. The administrative fees are then added on top.
A flat fee is paid to the pharmacy for dispensing the medication, and then a second fee of 15% or less is used to cover Express Scripts' services and shared among participating pharmacies to ensure they have a "reasonable profit."
Express Scripts said it is making the model available to a "broad network" of more than 65,000 retail pharmacies. It will apply to each drug on a plan sponsor's list, including generics, branded products and specialty medications, beginning Jan. 1.
“This new model differs from other pricing options where Express Scripts negotiates discounts with pharmacies to meet guaranteed rates for clients,” Kautzner said. “Express Scripts ClearNetwork is a simple pricing option that reinforces the value of our work to help consumers easily access the medications they need, while also shining a light on the root cause of high drug costs—drug manufacturers who set and raise prices.”
The ClearNetwork launch builds on new programs unveiled earlier this year, Express Scripts said. The pharmacy benefit manager, for example, announced ClearCareRx, which offers a greater transparency for its clients.
Express Scripts also said programs like Copay Assurance, SafeGuardRx, Embarc Benefit Protection and the Patient Assurance Program saved customers a combined $56 million in 2022.