As states continue to work through the lengthy backlog of Medicaid eligibility determinations, federal officials are urging them to do as much as possible to avoid large coverage losses.
Dan Tsai, deputy administrator of the Centers for Medicare & Medicaid Services (CMS) and director of the Center for Medicaid and CHIP Services, told reporters Wednesday that the agency’s goal is for states to meet and exceed federal requirements in limiting how many individuals lose healthcare coverage.
“We put out additional policy, levers and strategies for states that all get at reducing procedural termination rates, and our hope … is that all states take up every one of those policy flexibilities,” said Tsai during the press conference. “If all states do that, we will see a reduction in procedural terminations, and we will see an increase in the number of eligible people that maintain coverage. That is the bottom line and why we have been urging and partnering with states to … make sure they are following every federal requirement.
“We have been emphasizing it is not enough for states to simply follow federal minimums when it comes to Medicaid enrollments,” he added. “We are really asking every state to take up a whole host of policy waivers and strategies.”
Individuals currently enrolled through Medicaid or the Children’s Health Insurance Program (CHIP) generally go through annual renewal windows, which were put on pause during the COVID-19 public health emergency. Congress increased the federal matching rate for state Medicaid payments during the pandemic so long as states agreed to not drop anyone off Medicaid rolls. Eligibility redeterminations, after Medicaid disenrollments in February 2020, began April 1.
As of December, Congress requires states to submit monthly data to CMS and allows CMS to hold states accountable through enforcement tools. States are required to submit corrective action plans, otherwise CMS has the authority to impose fines.
“Now that states are resuming renewal, we are all laser-focused on ensuring that people can stay connected to health care coverage,” said CMS Administrator Chiquita Brooks-LaSure. “Prior to the pandemic, 17 million people would lose their Medicaid and CHIP coverage each year, including many kids and families who are still eligible, but got caught in red tape.”
KFF estimated that enrollment in Medicaid and CHIP has surged to nearly 95 million people, leaving Medicaid in an “unprecedented” situation, the agency said.
Brooks-LaSure pointed to work the Biden administration has completed in ensuring there are health plans available in the Affordable Care Act (ACA) marketplace that cost less than $10 a month, noting that there is an opportunity to keep people on coverage despite the churn rate.
“Business as usual in the past, included a lot of eligible people losing coverage for a period of time for procedural reasons, and then coming back onto coverage at a later point,” said Tsai. “That's not something we believe we should accept as the status quo.”
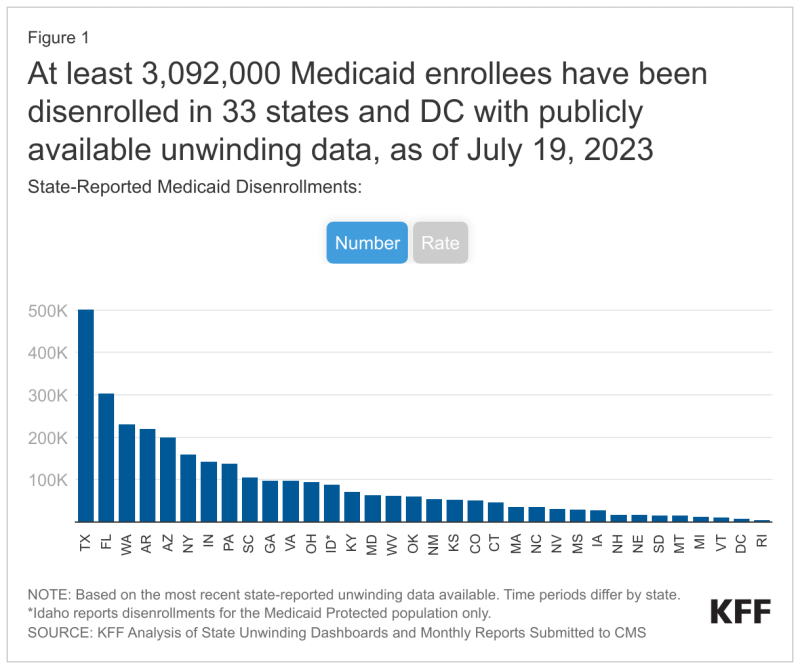
As of July 19, at least 3 million Medicaid members have been disenrolled from the program, according to from 33 states and the District of Columbia, KFF reported. Across all states with data, 74% of people had coverage terminated for procedural reasons such as outdated contact information or incomplete renewal packets. Many of these people could still be eligible for Medicaid or comparable coverage.
"We are very concerned, despite all the preparations and what we know has been a tremendous amount of work at the state level and in the community, about the level of terminations we are seeing across the country," Tsai said.
He said he is also concerned about the states who have not yet opted for Medicaid expansion because there will be people removed from Medicaid but will not have access to subsidized coverage.
South Dakota was the most recent holdout to expand Medicaid coverage under the ACA, leaving approximately 10 states remaining.
“I see this as a scenario where we all knew that trying to make sure that people retain coverage when we're at record levels of enrollment was going to be a difficult problem,” said Brooks-LaSure. “That's why we need everybody to do their part in this process. This is not a one-and-done effort, this is going to be a process.”
Ensuring compliance
If states do not meet federal requirements, CMS can require states to pause terminations, reinstate coverage and more—or risk losing the state’s enhanced federal funding. This requires states to stop disenrolling individuals for procedural reasons like not returning a renewal form, reinstate coverage, adopt strategies to address noncompliance and work toward full compliance.
Thirty-five states had approved mitigation plans from CMS as of April 1, according to a fact sheet provided by CMS.
CMS will offer technical assistance through adoption of new waivers and state plan amendments to help people maintain coverage or transition of coverage. They will also work with states to collaborate on managed care plans and providers, a decision the Department of Health and Human Services announced in June.
While most states are complying with requirements, the agency did list problems other states have encountered.
At least six states faced consequences when they did not provide enrollees Medicaid renewal forms, paused procedural terminations and reinstated coverage for people terminated inappropriately, along with issues regarding inaccurate data reporting standards.
CMS did not say which states are not currently in compliance, choosing to save that tactic for the future if needed.
“We’re not going to name states at this time,” said Brooks-LaSure. “At this moment, states have been working very collaboratively with us, and where we’ve found problems, they’ve been able to address them. However, if the day comes where they fail to comply. We won’t hesitate to make that information public.”
In the next few weeks, CMS expects to release data about Medicaid renewals in a state-by-state breakdown.