A coalition including the NAACP and other civil rights organizations released a scorecard Thursday grading each state on its policies handling the Medicaid unwinding period.
Only Hawaii earning a passing grade, while 25 states and the District of Columbia received an incomplete grade and the other 25 states received varying levels of failed grades.
More than 10 million Medicaid enrollees have been disenrolled nationally as of Nov. 8, following the end of pandemic-era Medicaid continuous eligibility requirements that required programs to keep beneficiaries enrolled.
“This report card shines the spotlight on the states who have not done the due diligence to ensure that every individual who's qualified to be on Medicaid actually has access to it,” said NAACP President and CEO Derrick Johnson during a press conference on Thursday.
In conjunction with public opinion research firm HIT Strategies and the NAACP, the states were measured on each state’s disenrollment status, Medicaid expansion status and procedural disenrollment rate to determine whether a state received a passing, incomplete or failing grade. To obtain a passing grade, states must have a procedural disenrollment rate at or below 5% or have voluntarily paused procedural disenrollments and be working toward an automatic renewal process. Failing grades were given to states with a procedural disenrollment greater than 5% that also had not paused procedural disenrollments or adopted Medicaid expansion.
Hawaii was celebrated with an "A" grade for adopting Medicaid expansion and choosing to pause procedural disenrollments. Florida was handed an "F-" score for showing no signs of addressing procedural disenrollment or adopting Medicaid expansion. States like Wisconsin, which have governors that advocate for Medicaid expansion but are blocked by state legislatures, were upgraded to "F+" scores.
“Medicaid unwinding is one of the biggest health issues our nation has had to reckon with this year,” said Juliet Choi, president and CEO of the Asian & Pacific Islander American Health Forum. “Failed leadership has brought us here.”
She added that states with the highest levels of termination rates have failed to invest in Medicaid infrastructure that could have avoided the crisis. As a result, governors have not properly cared for its underrepresented constituents.
“Governors have had time to plan for this,” said Eric Rodriguez, senior vice president of policy and advocacy for UnidosUS. “They've had resources from the federal government during the pandemic to get ready for this moment. And they have failed to live up to this moment and to serve families in the right ways.”
The coalition shared a recent report (PDF) showing that 54% of people losing Medicaid are estimated to come from communities of color and that children are not transitioning to Children’s Health Insurance Program (CHIP) once becoming unenrolled, suggesting that children are some of the most at-risk individuals.
“The fact of the matter is the American healthcare system has long failed Black Americans,” said Melicia Whitt-Glover, executive director for the Council on Black Health.
And often, beneficiaries’ coverage is terminated for procedural reasons or wrongfully canceled with little notice. The civil rights organizations said that up to 70% of disenrolled people could have been eligible for Medicaid but were denied coverage due to procedural reasons alone.
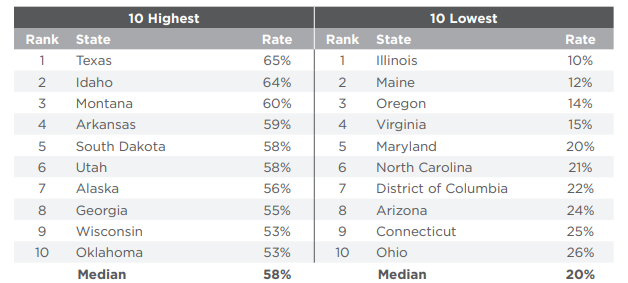
The 10 states with the highest termination rates spent $26 per beneficiary on Medicaid eligibility infrastructure during 2022, compared to $41 in the 10 states that were most successful in preventing Medicaid terminations. Poorly performing states limited funding, even while holding large budget surpluses, despite knowing unwinding would begin. Investment could’ve included hiring translators, upgrading computer systems, having functional and effective websites and funding call centers so they have the resources to hire staff.
Other solutions call for authorizing Medicaid managed care organizations to complete forms on behalf of members and allowing community organizations to speak directly with the states' eligibility systems to upload documents and troubleshoot problems.
“We know the power is in their [the governors’] hands and the same processes that have been used to disenroll vulnerable Americans can be used to automatically reenroll people who are eligible,” said Whitt-Glover. “We're not asking governors to reinvent the wheel.”
She called on states to pause procedural disenrollments, reenroll those who are eligible and then establish an automated renewal system.
Shavon Arline-Bradley, president and CEO of the National Council of Negro Women, said “paperwork is standing in the way of people.”
Even temporary health insurance gaps have been found to create poor health outcomes, as people are not treated for chronic illnesses, conditions go untreated and medical debt accumulates.
“One or two unpaid medical bills can ruin one’s credit, making home ownership more difficult … It is why we are united in saying today that states should pause this so-called unwinding,” said Marc Morial, president and CEO of the National Urban League.
In late September, the Centers for Medicare & Medicaid Services sent a letter to state health officials telling states they must provide 12 months of continuous coverage to children under age 19 on Medicaid and CHIP, effective Jan. 1. The coalition said state governments need to go several steps further by using Supplemental Nutrition Assistance Program data to find people with income low enough to qualify for Medicaid, as well as connecting Medicaid families to trained personnel that can complete paperwork for them.
The coalition includes the Asian & Pacific Islander American Health Forum, the Council on Black Health, the National Action Network, the NAACP, the National Coalition on Black Civic Participation/Black Women’s Roundtable, the National Council of Negro Women, the National Urban League and UnidosUS.