The Government Accountability Office flirted with the idea of requiring functional status information—such as whether patients could independently perform routine tasks such as bathing or dressing—in Medicare Advantage's risk adjustment models.
The reason? MA's risk adjustment models often underestimate spending for those with physical limitations while overestimating spending for those without such limitations.
But, recognizing the difficulty of collecting this information about patients in the program, the GAO ultimately stopped short in its report released Monday of actually recommending that the Centers for Medicare and Medicaid Services (CMS) do anything about taking that information into account.
That's an important oversight, as patients' functional status can have a big impact on their estimated healthcare costs. The 21st Century Cures Act, passed in December of 2016, sought to correct that oversight, directing GAO to explore the possibility of incorporating functional status information in risk adjustment models.
RELATED: CMS releases 32 quality measures under consideration for 2018
As GAO pointed out in its report, the current risk adjustment model formulas already account for the health status of beneficiaries, giving larger payouts to beneficiaries in poorer health to compensate for expected healthcare costs, the report said. But they systematically overestimate healthcare spending for patients with high functional status, and underestimates it for patients that can't function as easily. The agency estimated that 4 in 10 beneficiaries in 2016 had significant functional limitations.
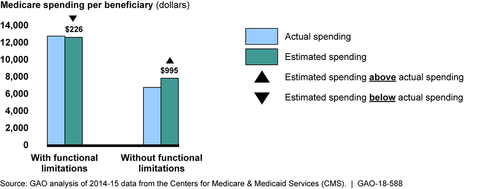
"These findings suggest that risk adjustment accuracy could be improved by accounting for functional status, which could, in turn, reduce any financial disadvantages plans may experience by enrolling beneficiaries with functional limitations," GAO said in the report (PDF).
Usually, at this point in a report, GAO would issue a recommendation to the responsible agency based on its findings. But in this case, the office seemed preemptively convinced that it would actually be unrealistic for CMS to incorporate functional status data in its formula.
GAO noted that functional status information isn't readily available, as only about a fourth of beneficiaries receive healthcare services in settings where this data is regularly recorded. As a result, collecting the data for all beneficiaries would mean a resource-intensive program for CMS, one that beneficiaries could see as an imposition.
RELATED: CMS floats Medicare Advantage payment tweaks that would boost insurers' risk scores
Furthermore, GAO worried that incorporating the information into risk adjustment formulas would set up a problematic incentive for MA plans to emphasize their beneficiaries' functional limits.
"Accounting for functional status in MA risk adjustment could give plans a financial incentive to identify functional limitations, which could pose a challenge related to overpayment. Such improvements in the identification of MA beneficiaries with functional limitations could result in these beneficiaries having higher risk scores—and appearing sicker—than beneficiaries in Medicare FFS with the same limitations, health conditions, and other characteristics," the report said.
As a result, GAO concluded without issuing a recommendation, leaving CMS and policymakers to dwell on the inefficiency.