In 2020, there has been an immense focus on infection control of the SARS-CoV-2 virus that causes the novel coronavirus (COVID-19) disease.
However, over the past decade, there has been a growing appreciation that environmental contamination of hospital surfaces promotes infection transmission for many pathogens. Shedding of any infectious pathogen is important. Numerous studies with epidemiologically important pathogens like multidrug resistant organisms (MDROs) such as methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), multidrug-resistant Acinetobacter, Candida auris and carbapenem-resistant Enterobacteriaceae have shown contamination of surfaces and the frequency of hand contamination correlates to the frequency of environmental contamination.
To prevent the spread of SARS-CoV-2 and other emerging MDROs, hospitals have implemented essential universal infection control strategies in their healthcare system that include wearing a mask, optimal hand hygiene and cleaning the environment.
Professional cleaning staff needs to be familiar with some of the most common and highly transmissible and infectious germs found in public spaces so they can implement infection prevention and control protocols designed to protect against them.
The common routes of transmission of healthcare-associated infections (HAIs) caused by MDROs are the source of transmission:
- By contamination of surfaces after terminal cleaning of isolation rooms resulting in a risk of acquisition by patients subsequently admitted to the same room;
- By contamination of surfaces in isolation rooms resulting in risk for contamination of health care personnel hands;
- By contamination of portable equipment; or
- By contamination of surfaces in rooms of unidentified carriers of healthcare-associated pathogens.
Elevating environmental disinfection strategies
This is why the implementation of environmental disinfection strategies to interrupt transmission to prevent the spread of infections is extremely important.
One study (PDF) suggests that environmental contamination plays a significant role in HAIs and in the unrecognized transmission of nosocomial pathogens during outbreaks. Several pathogens can persist in the environment for extended periods and serve as vehicles of transmission and dissemination in the hospital setting.
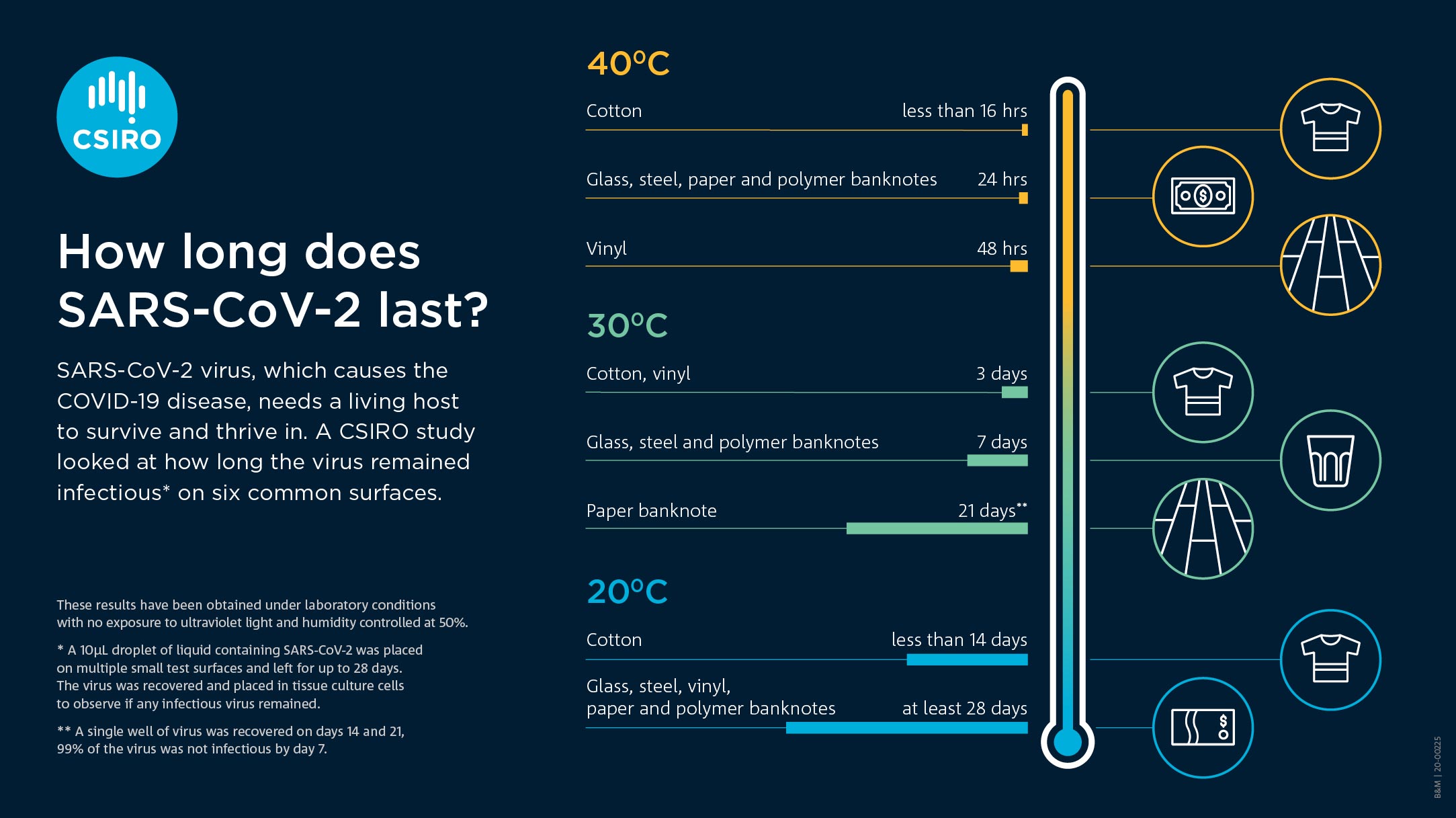
For example, coronaviruses (like SARS and SARS-CoV-2) can persist on inanimate surfaces— including metal, glass, or plastic for days (see photo by CSIRO) at different temperatures. This demonstrates SARS-CoV-2 can remain infectious for significantly longer time periods than generally considered possible and the role of environmental contamination and provides context for reinforcing the importance of hand hygiene and environmental decontamination for the prevention and control of cross-contamination.
It is so essential for optimal patient room cleaning to prevent healthcare-acquired pathogens because of the possibility of a patient admitted to a room where the previous occupant was colonized or infected with a MDRO had been shown to have a higher risk of acquiring the same MDRO. To reduce human error and provide optimal environmental cleaning; in 2017, a multicenter randomized controlled trial (PDF) evaluated the effect of enhanced disinfection strategies on acquisition and infection due to four target organisms (MRSA, VRE, multidrug-resistant Acinetobacter and Clostridioides difficile). By adding an ultraviolet (UV-C) device to a surface disinfectant protocol to decrease the risk of subsequent acquisition and infection by target organism, the study showed the efficacy of enhanced disinfection and confirms that the contaminated hospital environment is a modifiable risk factor for HAIs.
The role UV technology can play
Enhance cleaning and surface disinfectants with UV-C technology is a defense for COVID-19 as well. Over the summer, an article was published in Emerging Infectious Diseases on aerosol and surface distribution of SARS-CoV-2 in two hospital wards in Wuhan, China. The authors found contamination was greater in intensive care units than general wards. The virus was widely distributed on floors, computer mice, trashcans and sickbed handrails and was detected in the air about four meters from patients on these units.
However, an evidence-based approach for optimization of infection control and operating room management during the COVID-19 pandemic is based on confirmed modes of viral transmission: contact with contaminated environmental surfaces and aerosolization. For patient safety, effective strategies for attenuation of residual environmental contamination involve a combination of deep cleaning with surface disinfectants and UV-C in the fight against COVID-19.
COVID-19 spreads not only from person to person via close contact respiratory droplet and airborne transmission but also via contaminated surfaces.
For disease prevention, adding a robot-controlled non-contact UV-C surface disinfection can manage and address risks of infectious diseases. Since SARS-CoV-2 persists on inanimate surfaces, UV-C devices have been shown to reduce contamination on high-touch surfaces in hospitals. Instead of manual disinfection, which requires workforce mobilization and increases exposure risk to cleaning personnel, autonomous or remote-controlled disinfection robots could lead to an investment of fast, smooth-running and effective disinfection.
As more forward-thinking facilities are exploring how to fight infections with UV light, the Medline Newsroom took a closer look at disinfection and why experts say patients and staff can benefit when you don’t overlook the air.
Rosie Lyles, M.D., is the director of clinical affairs at Medline.