Most health plan executives believe physicians do not have the tools they need to succeed in value-based healthcare, and as a result, 67% of physicians and health plan executives said the U.S. still has a fee-for-service model, according to a recent study by Quest Diagnostics.
Quest said that although payment structures have changed in recent years to theoretically enable pricing based on health outcomes, the reporting requirements necessary to use those systems can be prohibitively strenuous—particularly if the practice or health system in question lacks a strong IT department.
"We're getting better at getting more of those quality measures outcome-based, but also culling them down," L. Patrick James, M.D., chief clinical officer of health plans and policy for medical affairs at Quest Diagnostics, told FierceHealthcare. So there's hundreds of these things out there, and many physicians are confused about what they should report for what type of arrangement.
"Maybe they have a value-based contract with X and maybe they're falling under MIPS for CMS, so the administrative burden for a physician in practice ... has become a huge burden for physicians to deal with the proliferation of quality measures," he said.
James hopes that if reporting burdens for payment systems like MIPS get less strenuous, as CMS has proposed, physicians will be enabled to better utilize those outcome-based pricing structures.
"If we would do the survey two weeks from now, the results might be a little bit different," James said. "[CMS] is getting rid of 34 of the quality measures for MIPS. So I think there is hope that this will get simplified, more consistent, more reproducible for reporting systems."
RELATED: A break for doctors: Trump administration wants to reduce reporting burden under MIPS
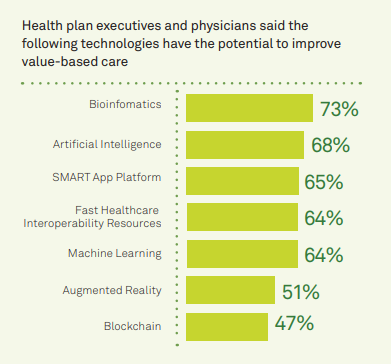
In the pursuit of delivering value-based healthcare, much has been made about the promise of new technologies. Robust Electronic Health Records (EHRs) should be able to cut down on redundant testing; bioinformatics should be able to give physicians better clues about a patient’s individual health; blockchain systems should be able to surmount interoperability challenges by sharing data across different health systems.
Yet these promises have yet to deliver, according to physicians in the survey. Just 39% of physicians said EHRs provide all the data they need for their patients, and 72% of all respondents agreed that doctors didn’t have all the information they needed about their patients.
Physicians were also significantly more bearish on the promise of these technologies than health plan executives; for instance, just 37% of physicians believe that blockchain has the potential to unlock healthcare value, compared with 66% of executives.
Quest Diagnostics argued that the discordance is mostly caused by a misalignment in expectations. As physicians learn what the technologies are capable of, they will embrace them as well.
"I think a lot of that is just awareness and knowledge. I think that as these tools get applied in practices going forward and they also take out some of the redundancy and administrative burden, I think physicians will be championing these technologies also," James said.
In all, James said the transition to value-based care will take place the more interoperability is realized.
“Measures that optimize EHRs, make data more accessible and insightful and reduce complexity of quality measurement are much-needed steps to accelerate this transition," he said in a statement. "First, however, it's clear that health plan executives and physicians need to better align around a shared vision of how technology and data can improve patient care."