Solera Health, a benefits network that connects patients, payers and physicians with a curated network of programs, has launched a new one-stop condition management platform.
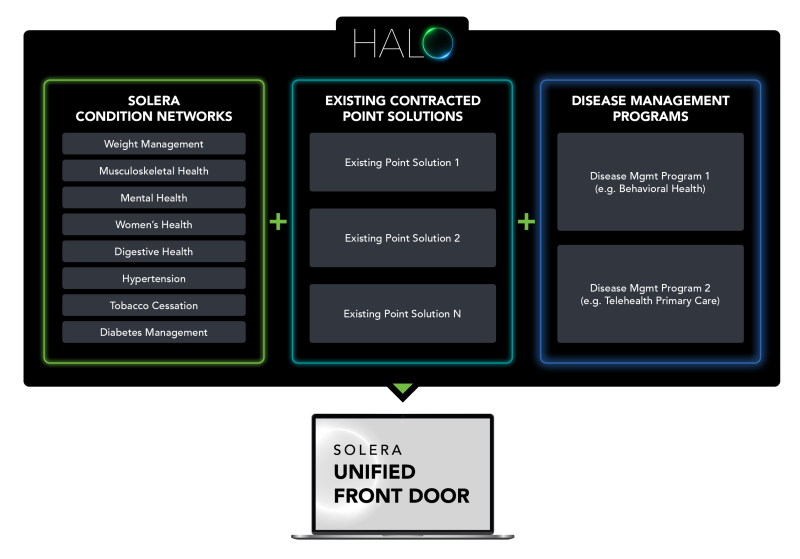
The HALO platform is an omni-condition management product that allows payers and employers to manage all Solera and non-Solera point solutions in a single user interface.
Payers and employers lack the time and resources to manage and compare dozens of contracted point solutions, resulting in a lack of vendor accountability and higher healthcare costs, Solera argues. The HALO platform aims to simplify that to help drive cost savings and best-fit interventions matched to patient preference and acuity level.
The platform’s integration eliminates the need to manage point solutions individually, Solera said. Its consolidated reporting dashboard can quickly assess the effectiveness of all programs side by side, potentially driving more informed decisions and better engagement in effective programs. With HALO, users can also organize relevant condition-specific resources for members and personalize the solutions they offer.
The integration represents the next stage of accountable care in digital health, executives said.
“Employers and payers have begun questioning the efficacy and cost of digital solutions. But the answer isn’t to throw the baby out with the bathwater,” Mary Langowski, CEO of Solera, said in a press release. “HALO addresses these challenges head-on—democratizing data for transparency and accountability, so we can not only create more opportunity for innovation in the industry, but also meaningfully and cost-effectively improve consumer health.”
Solera handles the most resource-intensive tasks associated with delivering complex programs to drive better health outcomes including claims processing, compliance, consumer engagement, eligibility checking, consumer matching and vendor management, according to the company.
Earlier this year, Solera partnered with Horizon Healthcare Services to offer customized healthcare to members. The effort’s initial focus is on launching programs for musculoskeletal problems, stress, sleep deprivation and weight management, among others. The companies believe the customized care will result in savings.