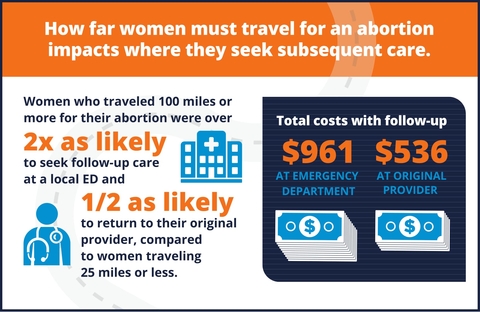
Women that travel long distances for an abortion are twice as likely to end up in the emergency room for follow-up care compared with those who were much closer to their provider at a higher cost to Medicaid. Researchers say those costs could be mitigated by improving access to telemedicine services.
Researchers with Advancing New Standards in Reproductive Health at the University of California, San Francisco, reviewed claims data from California’s Medicaid program, which covered nearly 40,000 abortions between 2011 and 2012. The results, published in Obstetrics & Gynecology, indicated that women who traveled 100 or more miles to have an abortion were much more likely to go to the ER for follow-up care compared with those that traveled less than 25 miles to their abortion provider.
“Increasing the number of rural Medicaid abortion providers by reimbursing for abortion care via telemedicine, and integrating abortion provision into primary care settings could increase access to abortion care for Medicaid recipients and improve care for women after they have an abortion,” he said.
RELATED: How telemedicine pulled one rural hospital back from the brink of bankruptcy
The study adds to an ongoing discussion about how telemedicine could improve access to care for patients living in rural parts of the country. In an editorial published in JAMA Internal Medicine, Mitchell H. Katz, M.D., the director of the Los Angeles County Department of Health Services, argued that expanding reimbursement for telemedicine would broadly improve access to specialty care services.
“For these visits to be financially sustainable the provider must be in a capitated system or there must be billing codes for such visits; at the moment, electronic consultations cannot generally be billed under Medicare, fee-for-service Medicaid, or private insurance,” he wrote.
A report issued earlier this year by NTCA–The Rural Broadband Association indicated that telehealth could save hospitals in rural parts of the country $81,000 annually on average, as well as significantly reduce costs for patients associated with lost work and travel.