We often view providing more healthcare as beneficial, but sometimes it can be harmful—physically, mentally and financially—for the patient and their family.
As members of the healthcare community, we’ve known about the problem of “low-value” care—care that provides no benefit, or where the risk of harm outweighs any potential benefits—for decades, and yet the healthcare industry has not been able to solve this systemic issue. Since 2011, the Health Care Cost Institute (HCCI), an independent, nonprofit research institute, has been working with health plans, government agencies, nonprofit healthcare organizations and academic institutions to bring awareness and action to the pervasive problem of low-value care.
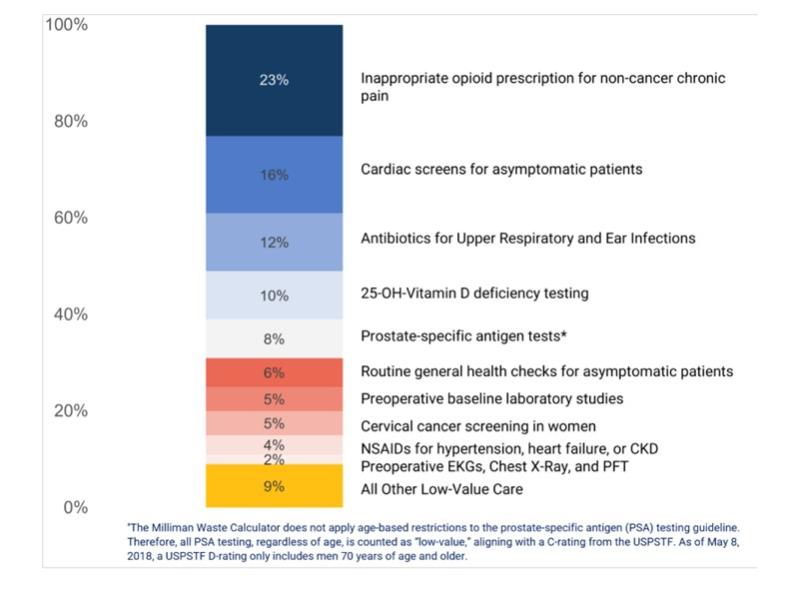
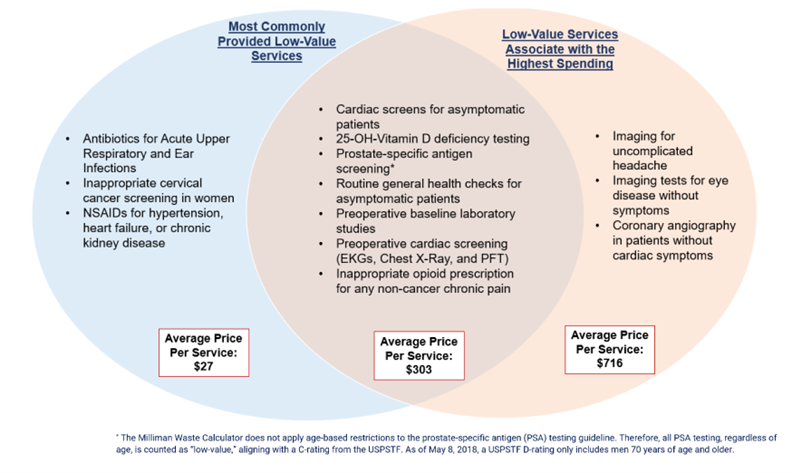
This month, HCCI shared in its “Right Care” report that “low-value care was highly concentrated among 10 services."
Affecting nearly 1 in 5 people in the study, the impact of low-value care had an average cost of up to $716 per service. The most commonly provided low-value service was inappropriate opioid prescriptions for non-cancer chronic pain. The highest spending low-value service was cardiac imaging screenings for patients without symptoms.
Why is it important?
According to a 2019 study, the total financial cost of low-value care for our entire U.S. health system is estimated to be up to $101.2 billion annually. However, the primary motivation for elimination of low-value care should be the prevention of harm to patients and burden on their families and caregivers.
Since Hippocrates, the medical profession has considered avoidance of harm a primary factor in driving care delivery. Provision of low-value care violates this core principle. This realization motivated the American Board of Internal Medicine Foundation to launch their "Choosing Wisely" campaign, educating care providers and recipients about the dangers of unnecessary care and prompting medical specialty societies to make targeted recommendations for reducing low-value care.
In today’s fiscally strained environment, the cost of low-value care cannot be ignored. HCCI’s "Right Care" report revealed that total spending on low-value care was 2.6%, and patients shouldered almost 20% of these costs in out-of-pocket spending.
However, the impact of low-value care is likely much greater than reported because unnecessary tests or treatments may lead to cascades of care, when patients are sent down a path of expensive services that lead to no visible benefit or even cause more harm. An unnecessary diagnostic test may come back with ambiguous results, leading to more tests in an attempt to clarify the initial results.
The patient and their family may become distressed as they get hospitalized for these additional tests—and, while in the hospital, is exposed to an infection. The physical, emotional and financial costs of this cascade of events often eclipses the cost of the original low-value service itself.
How do we address it?
Many of the necessary steps to reduce low-value care have begun. The Choosing Wisely campaign was a provider-led initiative that identified specific low-value services and promoted conversations between patients and clinicians. The Health Waste Calculator, used for this HCCI report, enables low-value care measurement at a broader health system level.
We must work with and across three key stakeholders—patients, providers and payers—of the healthcare ecosystem to reduce and eliminate low-value care.
Patients must ask questions
Patients need to be educated and empowered to ask and get answers to five key questions for any proposed medical intervention, especially those that are likely low-value services:
- Do I really need this test or procedure?
- What are the risks?
- Are there simpler, safer options?
- What happens if I don’t do anything?
- How much does it cost?
Providers must be accountable for the total cost of care
Providers and their healthcare teams need the time and should proactively answer all of the above and related questions. They need to be made aware of the total costs and downstream impact of low-value services they are prescribing.
We must also recognize that many providers reap financial rewards from delivering care in a fee-for-service model, even if the care has little or no value. Studies have reported that when providers are at risk for the total cost of care, they deliver less low-value care.
We need to change incentives to reward providers for the value of care rather than just the quantity of it.
Payers or health plans must drive incentives that reduce and eliminate low-value care
Health plans serve at the nexus of patients and providers, and they have information and data on both. They should work with providers and their employer and government customers, who represent their members, to create transparent measurement of low-value services and include its reduction in performance targets.
Furthermore, plans should work with employers and other customers who represent their members to design benefits packages and cost-sharing policies and strategies that discourage low-value care. For example, employers could challenge health plans at risk for 10 cents or more on the dollar for low-value services, and this may focus attention without imposing too much risk.
For decades, we recognize that healthcare costs are rising and unsustainable for this generation and the next. One area that is ripe for awareness and action is the reduction of low-value care. The time is now for all parties in the healthcare ecosystem— patients, providers and payers— to work together to assure that we receive the right care at the right time.
Kyu Rhee, M.D., is a senior scholar at the Stanford School of Medicine. Michael Chernew, Ph.D., is a health policy professor at Harvard Medical School. Katie Martin is the CEO of the Health Care Cost Institute.