What RAND researchers describe as “a remarkable transition in the U.S. health system from in-person to virtual care” occurred during the first year of the COVID-19 pandemic in 2020 for individuals seeking mental health services.
The study, published today in JAMA Health Forum, looks at data from about 5.1 million adults covered by commercial health insurance. The researchers examined data measuring county-level mental health utilization rates in all 50 states for adults 18 and older from Jan. 5, 2020, to Dec. 21, 2020, focusing on five diagnostic categories: major depressive disorder, anxiety disorders, bipolar disorder, adjustment disorder and post-traumatic stress disorder (PTSD).
The data were analyzed in April and May 2021.
The patients were grouped according to age, sex and mode of delivery for mental health services. The researchers found a more than 50% decline in in-person mental health care utilization among patients, which was entirely offset by rapid expansion in telehealth service utilization.
RAND researchers noted that while previous studies documented an increase in telehealth services during the pandemic, “to our knowledge, this is the first study to show that the magnitude of this increase (roughly a 16- to 20-fold increase in utilization) fully compensated for the decline in in-person care. For the 3 highest-prevalence diagnostic categories, we also found that service utilization continued to increase throughout 2020, primarily in the telehealth context.”
The use of telehealth to treat mental health will continue, Christopher M. Whaley, Ph.D., the study’s corresponding author, told Fierce Healthcare.
“Telehealth for behavioral health care has not declined in use over the course of the pandemic,” said Whaley. “This is in contrast to many other services, which saw an increase in telehealth care in the first few months of the pandemic, but then a rebound of in-person care. For behavioral health, telehealth has been sticky and use has remained constant.”

When COVID-19 was declared a national public health emergency (PHE) on March 13, 2020, the Department of Health and Human Services relaxed Health Insurance Portability and Accountability Act compliance regulations to promote broader adoption of telehealth, including use for mental health treatment. The PHE is set to expire in April, but the $1.7 trillion omnibus bill signed by President Joe Biden on Dec. 23, 2022, guarantees these flexibilities will continue for another two years.
According to the RAND study, the mean standard deviation for beneficiaries receiving help for depression before the pandemic stood at 11.66 per 10,000 enrollees each week. When COVID-19 struck, that declined to 6.44 beneficiaries per 10,000 enrollees. For anxiety disorder, 12.24 beneficiaries per 10,000 people dropped to 5.28; for bipolar disorder, 3.32 dropped to 1.81; for adjustment disorders, 12.14 dropped to 6.78; and for PTSD, 4.93 dropped to 2.
That’s when telehealth visits soared, with the lowest increase for bipolar disorder and the highest for anxiety disorder.
RAND researchers said they “were not able to assess quality of care and whether it differed between in-person and telehealth services. Although evidence from previous studies indicates that telemental health services are comparable with in-person services for conditions such as anxiety and depression, more evidence is required to establish quality of care in this and other samples."
One thing most can agree on: COVID-19 exacerbated the mental health problems of millions.
“The pandemic has been associated with decreased social interactions and physical exercise, threats to individuals’ employment and economic security, and an escalation in morbidity and mortality—all of which are likely to have contributed to widespread psychological distress,” the study said.
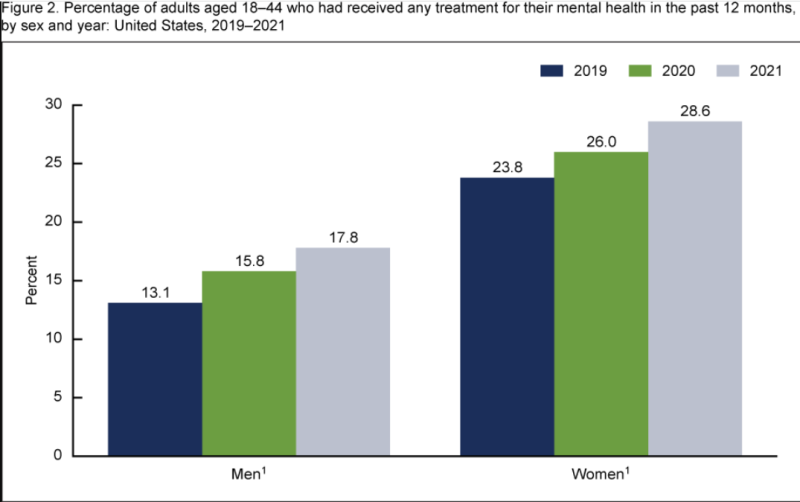
Women were more likely to seek help for anxiety disorders than men, which RAND researchers say may have to do with a greater comfort with telehealth among women. Also, women may have been under more stress, with many having to care for children not attending school.
Many had to put their careers on hold, becoming part of the "great resignation," the study noted.
The study also cites lower rates of telehealth for mental health services in rural counties, possibly as a result of those areas being low-income.
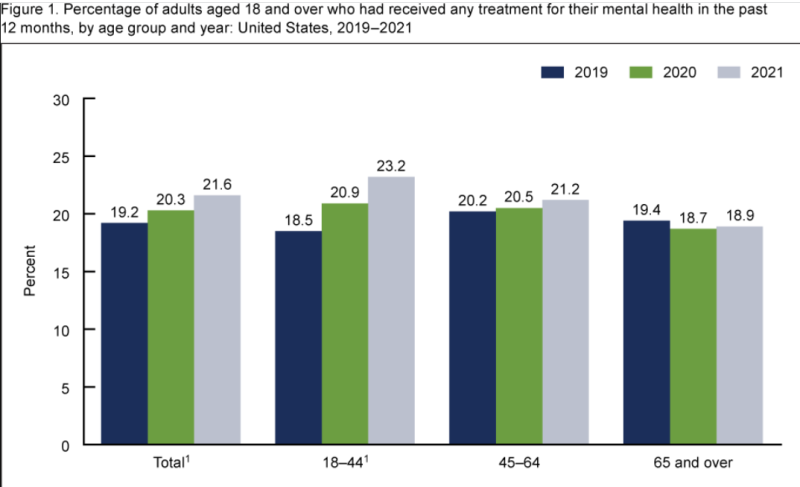
In addition, utilization rates for adults aged 46 or older were lower than that for younger adults, the study found.
“While this may be partly attributable to a lower prevalence of certain conditions among older adults, the consistency of this trend across diagnostic categories suggests that other factors may play a role, including the digital literacy and comfortability of older adults to use videoconferencing for communicating with healthcare professionals,” the study said.
Whaley, who is a health economist at RAND and professor at the RAND Pardee Graduate School, said that “the policy takeaway is that telehealth is a widely used modality for behavioral healthcare. Restricting telehealth use of behavioral health services would likely lead to reductions in behavioral health care.”